What is Revision Hip Replacement?
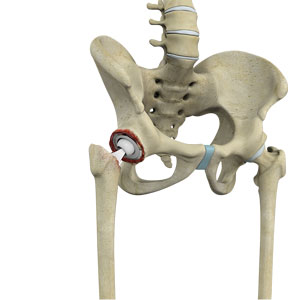
During total hip replacement, the damaged cartilage and bone are removed from the hip joint and replaced with artificial components. At times, hip replacement implants can wear out for various reasons and may need to be replaced with the help of a surgical procedure known as revision hip replacement surgery.
Revision hip replacement is a complex surgical procedure in which all or part of a previously implanted hip joint is replaced with a new artificial hip joint. Total hip replacement surgery is an option to relieve severe arthritis pain that limits your daily activities.
Indications for Revision Hip Replacement
Revision hip replacement is advised for the following conditions:
- Increasing pain in the affected hip
- Worn out plastic or polyethylene prosthesis
- Dislocation of previous implants
- Loosening of the femoral or acetabular component of the artificial hip joint
- Infection around the hip prosthesis, causing pain and fever
- Weakening of bone around the hip replacement (osteolysis)
Procedure of Revision Hip Replacement
Revision hip replacement surgery is performed under general anesthesia. During the procedure, your surgeon will make an incision over the hip to expose the joint. Then, the femur is dislocated from the acetabulum so that the old plastic liner and metal socket can be removed from the acetabulum.
After removal, the acetabulum is prepared using extra bone and wire mesh to make up for the socket space and shape. Then, the new metal shell is inserted into the socket using screws or special cement. A liner made of plastic, ceramic or metal is placed inside the metal socket.
To prepare the femoral component, the top of the femur bone is cut into several pieces to remove the implant. The segments of bone are cleaned and the new femoral implant is inserted into the femur either by a press fit or using bone cement. The segments of the femur and the femoral component are held together with surgical wires. Then the femoral head component made of metal or ceramic is placed on the femoral stem. All the new components are secured in place to form the new hip joint. The muscles and tendons around the new joint are repaired and the incision is closed.
Post-procedure Care for Revision Hip Replacement
After undergoing revision hip replacement, you must take special care to prevent the new joint from dislocating and to ensure proper healing. Some of the common precautions to be taken include:
- Avoid combined movement of bending your hip and turning your foot inwards because it can cause dislocation.
- Place a pillow between your legs while sleeping for 6 weeks.
- Never cross your legs or bend your hips past a right angle (90 degrees).
- Avoid sitting on a low chair.
- Avoid bending down to pick up things; instead, a grabber can be used to do so.
- Use an elevated toilet seat.
Risks of Revision Hip Replacement
As with any major surgical procedure, there are certain potential risks and complications involved with revision hip replacement surgery. The possible complications after revision hip replacement include:
- Infection
- Dislocation
- Fracture of the femur or pelvis
- Injury to nerves or blood vessels
- Formation of blood clots in the leg veins
- Leg length inequality
- Wearing of the hip prosthesis
- Failure to relieve pain
Related Topics:
- Mini-Posterior Hip Replacement
- Stryker Tripolar THA
- Robotic Total Hip Replacement
- Correction of a Failed Hip Replacement
- Correction of a Painful Hip Replacement
- Correction of a Loose Hip Replacement
- Outpatient Hip Replacement
- Physical Therapy for Hip
- Total Hip Replacement
- Minimally Invasive Total Hip Replacement
- Revision Hip Replacement
- Direct Superior Hip Replacement
- Robotic Assisted Hip Surgery

